Crohn's disease
2008/9 Schools Wikipedia Selection. Related subjects: Health and medicine
| Crohn's disease Classification and external resources |
|
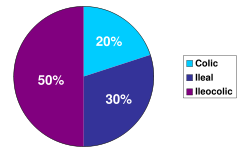
| The three most common sites of intestinal involvement in Crohn's disease are ileal, ileocolic and colonic. |
|
| ICD- 10 | K 50. |
| ICD- 9 | 555 |
| OMIM | 266600 |
| DiseasesDB | 3178 |
| MedlinePlus | 000249 |
| eMedicine | med/477 ped/507 radio/197 |
| MeSH | D003424 |
Crohn's disease (also known as regional enteritis) is an autoimmune disease, which can affect any part of the gastrointestinal tract from mouth to anus; as a result, the symptoms of Crohn's disease vary among afflicted individuals. The disease is characterized by areas of inflammation with areas of normal lining between in a symptom known as skip lesions. The main gastrointestinal symptoms are abdominal pain, diarrhea (which may be bloody, though this may not be visible to the naked eye), constipation, vomiting, weight loss or weight gain. Crohn's disease can also cause complications outside of the gastrointestinal tract such as skin rashes, arthritis, and inflammation of the eye.
The disease was independently described in 1904 by Polish surgeon Antoni Lesniowski and in 1932 by American gastroenterologist Burrill Bernard Crohn, for whom the disease was named. Crohn, along with two colleagues, described a series of patients with inflammation of the terminal ileum, the area most commonly affected by the illness. Crohn's disease affects between 400,000 and 600,000 people in North America. Prevalence estimates for Northern Europe have ranged from 27–48 per 100,000. Crohn's disease tends to present initially in the teens and twenties, with another peak incidence in the fifties to seventies, although the disease can occur at any age.
Although the cause of Crohn's disease is not known, it is believed to be an autoimmune disease that is genetically linked. The highest relative risk occurs in siblings, affecting males and females equally. Smokers are three times more likely to get Crohn's disease.
Unlike the other major types of IBD, there is no known drug based or surgical cure for Crohn's disease. Treatment options are restricted to controlling symptoms, putting and keeping the disease in remission and preventing relapse.
Classification
Crohn's disease is generally classified as an autoimmune disease. As it almost invariably affects the gastrointestinal tract, most gastroenterologists categorize the presenting disease by the affected areas. Ileocolic Crohn's disease, which affects both the ileum (the last part of the small intestine that connects to the large intestine) and the large intestine, accounts for fifty percent of cases. Crohn's ileitis, affecting the ileum only, accounts for thirty percent of cases, and Crohn's colitis, affecting the large intestine, accounts for the remaining twenty percent of cases, and may be particularly difficult to distinguish from ulcerative colitis. The disease can attack any part of the digestive tract, from mouth to anus. However, individuals affected by the disease rarely fall outside these three classifications, being affected in other parts of the gastrointestinal tract such as the stomach and esophagus. Crohn's disease may also be categorized by the behaviour of disease as it progresses. This was formalized in the Vienna classification of Crohn's disease. There are three categories of disease presentation in Crohn's disease: stricturing, penetrating, and inflammatory. Stricturing disease causes narrowing of the bowel which may lead to bowel obstruction or changes in the caliber of the feces. Penetrating disease creates abnormal passageways ( fistulae) between the bowel and other structures such as the skin. Inflammatory disease (or non-stricturing, non-penetrating disease) causes inflammation without causing strictures or fistulae.
Symptoms
Many people with Crohn's disease have symptoms for years prior to the diagnosis. The usual onset is between 15 and 30 years of age but can occur at any age. Because of the patchy nature of the gastrointestinal disease and the depth of tissue involvement, initial symptoms can be more vague than with ulcerative colitis. People with Crohn's disease will go through periods of flare-ups and remission.
Gastrointestinal symptoms
Abdominal pain may be the initial symptom of Crohn's disease. The pain is commonly cramp-like and may be relieved by defecation. It is often accompanied by diarrhea, which may or may not be bloody, though diarrhea is not uncommon especially in those who have had surgery. People who have had surgery or multiple surgeries often end up with short bowel syndrome of the gastrointestinal tract. The nature of the diarrhea in Crohn's disease depends on the part of the small intestine or colon that is involved. Ileitis typically results in large-volume watery feces. Colitis may result in a smaller volume of feces of higher frequency. Fecal consistency may range from solid to watery. In severe cases, an individual may have more than 20 bowel movements per day and may need to awaken at night to defecate. Visible bleeding in the feces is less common in Crohn's disease than in ulcerative colitis, but may be seen in the setting of Crohn's colitis. Bloody bowel movements are typically intermittent, and may be bright or dark red in colour. In the setting of severe Crohn's colitis, bleeding may be copious. Flatulence and bloating may also add to the intestinal discomfort.
Symptoms caused by intestinal stenosis are also common in Crohn's disease. Abdominal pain is often most severe in areas of the bowel with stenoses. In the setting of severe stenosis, vomiting and nausea may indicate the beginnings of small bowel obstruction. Crohn's disease may also be associated with primary sclerosing cholangitis, a type of inflammation of the bile ducts.
Perianal discomfort may also be prominent in Crohn's disease. Itchiness or pain around the anus may be suggestive of inflammation, fistulization or abscess around the anal area or anal fissure. Perianal skin tags are also common in Crohn's disease. Fecal incontinence may accompany peri-anal Crohn's disease. At the opposite end of the gastrointestinal tract, the mouth may be affected by non-healing sores ( aphthous ulcers). Rarely, the esophagus, and stomach may be involved in Crohn's disease. These can cause symptoms including difficulty swallowing ( odynophagia), upper abdominal pain, and vomiting.
Systemic symptoms
Crohn's disease, like many other chronic, inflammatory diseases, can cause a variety of systemic symptoms. Among children, growth failure is common. Many children are first diagnosed with Crohn's disease based on inability to maintain growth. As Crohn's disease may manifest at the time of the growth spurt in puberty, up to 30% of children with Crohn's disease may have retardation of growth. Fever may also be present, though fevers greater than 38.5 ˚C (101.3 ˚F) are uncommon unless there is a complication such as an abscess Among older individuals, Crohn's disease may manifest as weight loss. This is usually related to decreased food intake, since individuals with intestinal symptoms from Crohn's disease often feel better when they do not eat and might lose their appetite. People with extensive small intestine disease may also have malabsorption of carbohydrates or lipids, which can further exacerbate weight loss.
Extraintestinal symptoms
In addition to systemic and gastrointestinal involvement, Crohn's disease can affect many other organ systems. Inflammation of the interior portion of the eye, known as uveitis, can cause eye pain, especially when exposed to light ( photophobia). Inflammation may also involve the white part of the eye ( sclera), a condition called episcleritis. Both episcleritis and uveitis can lead to loss of vision if untreated.
Crohn's disease is associated with a type of rheumatologic disease known as seronegative spondyloarthropathy. This group of diseases is characterized by inflammation of one or more joints ( arthritis) or muscle insertions ( enthesitis). The arthritis can affect larger joints such as the knee or shoulder or may exclusively involve the small joints of the hand and feet. The arthritis may also involve the spine, leading to ankylosing spondylitis if the entire spine is involved or simply sacroiliitis if only the lower spine is involved. The symptoms of arthritis include painful, warm, swollen, stiff joints and loss of joint mobility or function.
Crohn's disease may also involve the skin, blood, and endocrine system. One type of skin manifestation, erythema nodosum, presents as red nodules usually appearing on the shins. Erythema nodosum is due to inflammation of the underlying subcutaneous tissue and is characterized by septal panniculitis. Another skin lesion, pyoderma gangrenosum, is typically a painful ulcerating nodule. Crohn's disease also increases the risk of blood clots; painful swelling of the lower legs can be a sign of deep venous thrombosis, while difficulty breathing may be a result of pulmonary embolism. Autoimmune hemolytic anaemia, a condition in which the immune system attacks the red blood cells, is also more common in Crohn's disease and may cause fatigue, pallor, and other symptoms common in anaemia. Clubbing, a deformity of the ends of the fingers, may also be a result of Crohn's disease. Finally, Crohn's disease may cause osteoporosis, or thinning of the bones. Individuals with osteoporosis are at increased risk of bone fractures.
Crohn's disease can also cause neurological complications (reportedly in up to 15% of patients). The most common of these are seizures, stroke, myopathy, peripheral neuropathy, headache and depression.
Crohn's patients often also have issues with Small bowel bacterial overgrowth syndrome, which has similar symptoms.
Complications
Crohn's disease can lead to several mechanical complications within the intestines, including obstruction, fistulae, and abscesses. Obstruction typically occurs from strictures or adhesions which narrow the lumen, blocking the passage of the intestinal contents. Fistulae can develop between two loops of bowel, between the bowel and bladder, between the bowel and vagina, and between the bowel and skin. Abscesses are walled off collections of infection, which can occur in the abdomen or in the perianal area in Crohn's disease sufferers.
Crohn's disease also increases the risk of cancer in the area of inflammation. For example, individuals with Crohn's disease involving the small bowel are at higher risk for small intestinal cancer. Similarly, people with Crohn's colitis have a relative risk of 5.6 for developing colon cancer. Screening for colon cancer with colonoscopy is recommended for anyone who has had Crohn's colitis for eight years, or more.
Individuals with Crohn's disease are at risk of malnutrition for many reasons, including decreased food intake and malabsorption. The risk increases following resection of the small bowel. Such individuals may require oral supplements to increase their caloric intake, or in severe cases, total parenteral nutrition (TPN). Most people with moderate or severe Crohn's disease are referred to a dietitian for assistance in nutrition.
Crohn's disease can cause significant complications including bowel obstruction, abscesses, free perforation and hemorrhage.
Crohn's disease can be problematic during pregnancy, and some medications can cause adverse outcomes for the fetus or mother. Consultation with an obstetrician and gastroenterologist about Crohn's disease and all medications allows preventative measures to be taken. In some cases, remission can occur during pregnancy. Certain medications can also impact sperm count or may otherwise adversely affect a man's ability to conceive.
Cause
The exact cause of Crohn's disease is unknown. However, environmental and genetic factors have been invoked in the pathogenesis of the disease. Research has indicated that Crohn's disease has a strong genetic link. The disease runs in families and those with a sibling with the disease are 30 times more likely to develop it than the normal population. Ethnic background is also a risk factor. Until very recently, whites and European Jews accounted for the vast majority of the cases in the United States, and in most industrialized countries, this demographic is still true. However, the European commission makes an interesting point:
A review of the literature suggests that Crohn’s disease is more prevalent in Western populations with northern European and Anglo-Saxon ethnic derivation, than in populations of southern Europe, Asia and Africa. However, when the Asian people migrate to urban-industrial societies of the West, they become as susceptible to the disease as the population of their host countries, suggesting environmental factors in the aetiology of Crohn’s disease143.
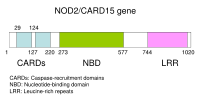
Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity. In earlier studies, only two genes were linked to Crohn's, but scientists now believe there are over eight genes that show genetics play a role in the disease, either directly through causation or indirectly as with a spurious relationship.
A handful of cases of Crohn's disease cases were reported at the turn of the 20th century, but since then, the disease has continued to increase in prevalence dramatically. Some argue that this increase has been the result of a genetic shift in the population caused by conditions favoring individuals carrying the genes linked with the disease. These conditions could be a lower infant mortality rate or better health care in the nations that have the highest incidence of disease (industrialized nations). Another explanation is that modern industrial practices have given rise to increased disease prevalence via infectious diseases. A common recurrent theory is that a specific species of Mycobacterium, Mycobacterium avium subspecies paratuberculosis, is responsible for both Johne's disease and Crohn's disease, and modern industrial farming practices have led to the spread of Mycobacterium avium subspecies paratuberculosis.
Others argue that Crohn's disease is caused by a combination of environmental and genetic factors. Many environmental factors have also been hypothesized as causes or risk factors for Crohn's disease. Proven environmental risk factors include living in an industrialized country, smoking, and living in an urban area. Diets high in sweet, fatty or refined foods may also play a role. A retrospective Japanese study found that those diagnosed with Crohn's disease had higher intakes of sugar, fat, fish and shellfish than controls prior to diagnosis. A similar study in Israel also found higher intakes of fats (especially chemically modified fats) and sucrose, with lower intakes of fructose and fruits, water, potassium, magnesium and vitamin C in the diets of Crohn's disease sufferers before diagnosis, and cites three large European studies in which sugar intake was significantly increased in people with Crohn's disease compared with controls. The most common forms of microparticles include titanium dioxide, aluminosilicates, anatase, calcium phosphate, and soil residue. These substances are ubiquitous in processed food and most toothpastes and lip glosses. Soil residue is found on fresh fruits and vegetables unless carefully removed.
Smoking has been shown to increase the risk of the return of active disease, or "flares". The introduction of hormonal contraception in the United States in the 1960s is linked with a dramatic increase in the incidence rate of Crohn's disease. Although a causal linkage has not been effectively shown, there remain fears that these drugs work on the digestive system in similar ways to smoking.
Additionally, many in the scientific community believe that early childhood exposure to illness is necessary to the creation of a proper immune system for those with the genetic susceptibility for Crohn's Disease. Higher incidences of Crohn's Disease are associated with cleaner living conditions. Throughout the early and mid-20th century in the United States, the disease was strongly associated with upper-class populations, and today the disease does not yet exist in the many Third World countries, despite the fact that it occurs in all races. CD is also associated with first born and single children (because they would have less exposure to childhood illness from siblings) and in populations that have low incidences of gastric cancer. Gastric cancer is most often caused by the bacterium Helicobacter pylori that flourishes in cramped and unsanitary conditions.
Abnormalities in the immune system have often been invoked as being causes of Crohn's disease. It has been hypothesized that Crohn's disease involves augmentation of the Th1 of cytokine response in inflammation. The most recent gene to be implicated in Crohn's disease is ATG16L1, which may reduce the effectiveness of autophagy, and hinder the body's ability to attack invasive bacteria.
A variety of pathogenic bacteria were initially suspected of being causative agents of Crohn's disease and many groups still suspect Mycobacterium avium subspecies paratuberculosis. However, the consensus of many health care professionals for several years has been that a variety of microorganisms are simply taking advantage of their host's weakened mucosal layer and inability to clear bacteria from the intestinal walls, both symptoms of the disease. Some studies have linked Mycobacterium avium subsp. paratuberculosis to Crohn's disease, in part because it causes a very similar disease, Johne's disease, in cattle. The mannose bearing antigens, mannins, from yeast may also elicit pathogenic anti saccharomyces cerevisiae antibodies. Studies have linked specific strains of enteroadherent E. coli to the disease. Still this relationship and evidence of contributions by other species remains controversial. And more recently a relationship between MAP and E. coli has been uncovered. Scientists at the university of Liverpool have discovered that "Mycobacteria release a complex molecule containing a sugar, called mannose. This molecule prevents a type of white blood cells, called macrophages, from killing internalized E.Coli.”
Some scientific studies and court rulings have posited that Accutane is a probable cause of IBD, a group of diseases including Crohn's Disease and Ulcerative colitis, in some individuals. Three cases in the United States have gone to trial thus far, with all three resulting in multi-million dollar judgments against the makers of isotretinoin; there are an additional 425 cases pending.
Pathophysiology
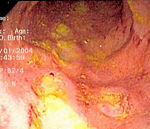
At the time of colonoscopy, biopsies of the colon are often taken in order to confirm the diagnosis. There are certain characteristic features of the pathology seen that point toward Crohn's disease. Crohn's disease shows a transmural pattern of inflammation, meaning that the inflammation may span the entire depth of the intestinal wall. Grossly, ulceration is an outcome seen in highly active disease. There is usually an abrupt transition between unaffected tissue and the ulcer. Under a microscope, biopsies of the affected colon may show mucosal inflammation. This inflammation is characterized by focal infiltration of neutrophils, a type of inflammatory cell, into the epithelium. This typically occurs in the area overlying lymphoid aggregates. These neutrophils, along with mononuclear cells, may infiltrate into the crypts leading to inflammation (crypititis) or abscess (crypt abscess). Granulomas, aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. The granulomas of Crohn's disease do not show "caseation", a cheese-like appearance on microscopic examination that is characteristic of granulomas associated with infections such as tuberculosis. Biopsies may also show chronic mucosal damage as evidenced by blunting of the intestinal villi, atypical branching of the crypts, and change in the tissue type ( metaplasia). One example of such metaplasia, Paneth cell metaplasia, involves development of Paneth cells (typically found in the small intestine) in other parts of the gastrointestinal system.
Diagnosis
The diagnosis of Crohn's disease can sometimes be challenging, and a number of tests are often required to assist the physician in making the diagnosis. Even with a full battery of tests it may not be possible to diagnose Crohn's with complete certainty; a colonoscopy is approximately 70% effective in diagnosing the disease with further being less effective. Disease in the small bowel is particularly difficult to diagnose as a traditional colonoscopy only allows access to the colon and lower portions of the small intestines; introduction of the Capsule endoscopy aids in endoscopic diagnosis.
Endoscopy
A colonoscopy is the best test for making the diagnosis of Crohn's disease as it allows direct visualization of the colon and the terminal ileum, identifying the pattern of disease involvement. Occasionally, the colonoscope can travel past the terminal ileum but it varies from patient to patient. During the procedure, the gastroenterologist can also perform a biopsy, taking small samples of tissue for laboratory analysis which may help confirm a diagnosis. As 30% of Crohn's disease involves only the ileum, cannulation of the terminal ileum is required in making the diagnosis. Finding a patchy distribution of disease, with involvement of the colon or ileum but not the rectum, is suggestive of Crohn's disease, as are other endoscopic stigmata.The utility of capsule endoscopy for this, however, is still uncertain.
Radiologic tests
A small bowel follow-through may suggest the diagnosis of Crohn's disease and is useful when the disease involves only the small intestine. Because colonoscopy and gastroscopy allow direct visualization of only the terminal ileum and beginning of the duodenum, they cannot be used to evaluate the remainder of the small intestine. As a result, a barium follow-through x-ray, wherein barium sulfate suspension is ingested and fluoroscopic images of the bowel are taken over time, is useful for looking for inflammation and narrowing of the small bowel. Barium enemas, in which barium is inserted into the rectum and fluoroscopy used to image the bowel, are rarely used in the work-up of Crohn's disease due to the advent of colonoscopy. They remain useful for identifying anatomical abnormalities when strictures of the colon are too small for a colonoscope to pass through, or in the detection of colonic fistulae.
CT and MRI scans are useful for evaluating the small bowel with enteroclysis protocols.They are additionally useful for looking for intra-abdominal complications of Crohn's disease such as abscesses, small bowel obstruction, or fistulae. Magnetic resonance imaging (MRI) are another option for imaging the small bowel as well as looking for complications, though it is more expensive and less readily available
Blood tests
A complete blood count may reveal anaemia, which may be caused either by blood loss or vitamin B12 deficiency. The latter may be seen with ileitis because vitamin B12 is absorbed in the ileum. Erythrocyte sedimentation rate, or ESR, and C-reactive protein measurements can also be useful to gauge the degree of inflammation. It is also true in patient with ilectomy done in response to the complication. Another cause of anaemia is anaemia of chronic disease, characterized by its microcytic and hypochromic anaemia. There can be various reasons for anaemia, including medication used in treatment of inflammatory bowel disease like azathioprine which can lead to cytopenia and sulfasalazine which can also result in folate malabsorption, etc. Testing for anti- Saccharomyces cerevisiae antibodies (ASCA) and anti-neutrophil cytoplasmic antibodies (ANCA) has been evaluated to identify inflammatory diseases of the intestine and to differentiate Crohn's disease from ulcerative colitis.
Comparison with ulcerative colitis
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Terminal ileum involvement | Commonly | Seldom |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually |
| Involvement around the anus | Common | Seldom |
| Bile duct involvement | No increase in rate of primary sclerosing cholangitis | Higher rate |
| Distribution of Disease | Patchy areas of inflammation (Skip lesions) | Continuous area of inflammation |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers | Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues | Shallow, mucosal |
| Fistulae | Common | Seldom |
| Stenosis | Common | Seldom |
| Autoimmune disease | Widely regarded as an autoimmune disease | No consensus |
| Cytokine response | Associated with Th1 | Vaguely associated with Th2 |
| Granulomas on biopsy | Can have granulomas | Granulomas uncommon |
| Surgical cure | Often returns following removal of affected part | Usually cured by removal of colon |
| Smoking | Higher risk for smokers | Lower risk for smokers |
Treatment
Currently there is no cure for Crohn's disease and remission may not be possible or prolonged if achieved; in cases where remission is possible, relapse can be prevented and symptoms controlled with medication, lifestyle changes and in some cases, surgery. Adequately controlled, Crohn's disease may not significantly restrict daily living. Treatment for Crohn's disease is only when symptoms are active and involve first treating the acute problem, then maintaining remission.
Medication
Acute treatment uses medications to treat any infection (normally antibiotics) and to reduce inflammation (normally aminosalicylate anti-inflammatory drugs and corticosteroids). When symptoms are in remission, treatment enters maintenance with a goal of avoiding the recurrence of symptoms. Prolonged use of corticosteroids has significant side-effects; as a result they are generally not used for long-term treatment. Alternatives include aminosalicylates alone, though only a minority are able to maintain the treatment, and many require immunosuppressive drugs.
Medications used to treat the symptoms of Crohn's disease include 5-aminosalicylic acid (5-ASA) formulations, prednisone, immunomodulators such as azathioprine, mercaptopurine, methotrexate, infliximab, adalimumab and natalizumab.
Lifestyle changes
Certain lifestyle changes can reduce symptoms, including dietary adjustments, proper hydration and smoking cessation.
Surgery
Crohn's cannot be cured by surgery, though it is used when partial or a full blockage of the intestine occurs. Surgery may also be required for complications such as obstructions, fistulas and/or abscesses, or if the disease does not respond to drugs within a reasonable time. After the first surgery, Crohn's usually shows up at the site of the resection though it can appear in other locations. After a resection, scar tissue builds up which causes strictures. A stricture is when the intestines becomes too small to allow excrement to pass through easily which can lead to a blockage. After the first resection, another resection may be necessary within five years. For patients with an obstruction due to a stricture, two options for treatment are strictureplasty and resection of that portion of bowel. There is no statistical significance between strictureplasty alone versus strictureplasty and resection in cases of duodenal involvement. In these cases, re-operation rates were 31% and 27%, respectively, indicating that strictureplasty is a safe and effective treatment for selected patients with duodenal involvement.
Short bowel syndrome (SBS, also short gut syndrome or simply short gut) can be caused by the surgical removal of the small intestines. It usually develops if a person has had half or more of their small intestines removed. Diarrhea is the main symptom of short bowel syndrome though other symptoms may include cramping, bloating and heartburn. Short bowel syndrome is treated with changes in diet, intravenous feeding, vitamin and mineral supplements and treatment with medications.
Prospective treatments
Researchers at University College London have questioned the wisdom of suppressing the immune system in Crohn's, as the problem may be an under-active rather than an over-active immune system: their study found that Crohn's patients showed an abnormally low response to an introduced infection, marked by a poor flow of blood to the wound, and the response improved when the patients were given sildenafil.
Recent studies using helminthic therapy or hookworms to treat Crohn's Disease and other (non-viral) auto-immune diseases seem to yield promising results.
A single, small, uncontrolled trial of patients with mild Crohn's on stable medications suggested improvement with low dose naltrexone therapy.
A recent small double-blind, placebo-controlled study conducted in Germany found grand wormwood to have a steroid-sparing effect with the result that 18/20 wormwood receiving patients were able to taper steroid medication while maintaining a steady improvement in CD symptoms.
Prognosis
Crohn's disease is a chronic condition for which there is currently no cure. It is characterised by periods of improvement followed by episodes when symptoms flare up. With treatment, most people achieve a healthy height and weight, and the mortality rate for the disease is low. Crohn's disease is associated with an increased risk of small bowel and colorectal carcinoma.
Epidemiology
The incidence of Crohn's disease has been ascertained from population studies in Norway and the United States and is similar at 6 to 7.1:100,000. Crohn's disease is more common in northern countries, and shows a higher preponderance in northern areas of the same country. The incidence of Crohn's disease is thought to be similar in Europe but lower in Asia and Africa. It also has a higher incidence in Ashkenazi Jews.
Crohn's disease has a bimodal distribution in incidence as a function of age: the disease tends to strike people in their teens and 20s, and people in their 50s through to their 70s, and ages in between due to not being diagnosed with Crohn's and being diagnosed instead with irritable bowel syndrome IBS. It is rarely diagnosed in early childhood. It usually strikes females more than males. Parents, siblings or children of people with Crohn's disease are 3 to 20 times more likely to develop the disease. Twin studies show a concordance of greater than 55% for Crohn's disease.
History
Inflammatory bowel diseases were described by Giovanni Battista Morgagni (1682-1771), by Polish surgeon Antoni Leśniowski in 1904 (leading to the use of the eponym "Leśniowski-Crohn disease" in Poland) and by Scottish physician T. Kennedy Dalziel in 1913.
Burrill Bernard Crohn, an American gastroenterologist at New York City's Mount Sinai Hospital, described fourteen cases in 1932, and submitted them to the American Medical Association under the rubric of "Terminal ileitis: A new clinical entity". Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer published the case series as "Regional ileitis: a pathologic and clinical entity".